Does My Child Have CP or Not? Complete Guide for Early Warning Signs of Cerebral Palsy

Early Warning Signs of Cerebral Palsy in Infants Birth to 12 Months: A Complete Resource Guide for Proactive Parents, Caregivers, and Professionals
Cerebral palsy (CP) is a broad term used to describe a group of disorders that affect a person's ability to move, maintain balance, and control their posture. It is the most common motor disability in childhood, occurring in approximately 1 in 345 children (1). This resource guide is designed to empower proactive parents with knowledge about the early warning signs of cerebral palsy in infants from birth to 12 months old. Early identification of potential signs, coupled with prompt intervention, can have a profound impact on a child's development and overall well-being and getting on top of their optimal development despite life-long challenges that may be inevitable.
Please note that the wording in red is important insights about Cerebral Palsy (CP) by Movement Lesson.
Blog Summary:
- What is Cerebral Palsy
- Types of Cerebral Palsy
- Disclaimer
- Recognizing the Early Warning Signs
- List of Early Warning Signs of CP
- Communicating With Your Doctor
- How Is Cerebral Palsy Diagnosed?
- Diagnostic Tools and Tests
- When Will The Doctor Start the Diagnostic Process?
- How Much Delay Does a Child Need To Have?
- When Medical Help May Not Be Offered
-
Believed Benefits of Traditional Early Intervention
-
Believed Benefits of Early Physiotherapy
- The Importance of Active Movement
-
- Believed Benefits of Movement Lesson Early Intervention
- Optimal Movement Development, and Independence for Best Quality of Life
-
Traditional Plan of Action Following a Cerebral Palsy Diagnosis
-
The Movement Lesson™ Optimal Plan of Action For Risk of Cerebral Palsy (CP) Diagnosis
- Things Parents Can Do NOW To Help Their Child Thrive
- Resources for CP Parents
- Works Cited
What is Cerebral Palsy?
Cerebral palsy is not a single condition but rather a group of neurological disorders that affect muscle movement and coordination. These disorders originate from damage to or abnormalities within the developing brain, most often before birth (2). This damage disrupts the brain's ability to control movement, maintain posture, and achieve balance. It's important to note that in many instances, the exact cause of cerebral palsy remains unknown (4).
The term "cerebral" pertains to the brain, while "palsy" refers to impaired motor function (3). Sometimes, the brain regions responsible for muscle control do not develop as expected during fetal growth. In other cases, brain damage may occur before, during, or after birth (3). While cerebral palsy is a lifelong condition, it's crucial to understand that it is a non-progressive disorder. This means that the brain damage itself does not worsen over time (5).
Types of Cerebral Palsy
Cerebral palsy can be categorized into different types based on the specific movement disorders involved (6):
- Spastic Cerebral Palsy: This is the most common type, affecting approximately 80% of children with CP (6). It is characterized by stiff muscles and exaggerated reflexes, which can make movement difficult.
- Dyskinetic Cerebral Palsy: This type involves involuntary movements, such as tremors or writhing motions, that a child cannot control.
- Ataxic Cerebral Palsy: This type affects balance and coordination, making it challenging for children to perform precise movements.
- Mixed Cerebral Palsy: Some children may have a combination of different types of cerebral palsy.
Disclaimer
The information provided in this blog is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your child's health or treatment.
This blog is not intended to diagnose, treat, or cure any medical condition, nor is it a substitute for professional medical advice. Always seek the advice of your pediatrician or other qualified healthcare provider with any questions you may have regarding a medical condition.
Individual results may vary, and this blog does not guarantee any specific outcomes.
Recognizing the Early Warning Signs
Optimal infant development is crucial, and recognizing potential warning signs of cerebral palsy (CP) is essential for early intervention. Here's what you need to know to advocate for your child:
List of Early Warning Signs of CP:
While some signs may be present at birth, others emerge as the baby grows. Here are some key things to watch for in infants 0-12 months old. Please note that the answer in GREEN indicates a lower risk for CP, and the answer in BLUE indicates a higher risk of CP. DISCLAIMER: THIS IS NOT A DIAGNOSTIC TOOL FOR CP:
- Trauma: Did your baby suffer from birth trauma, surgical delivery, NICU (Neonatal Intensive Care Unit), surgery, or prolonged hospitalization (this could also include (forceps used, vacuum used, emergency delivery, brain damage, oxygen deprivation, cord wrapped around the neck)? Yes / No
- Gravity: Do your baby's movements counter-oppose of gravity? Yes / No
- Abnormal Muscle Tone: Does your baby feel unusually stiff or floppy (7)? Yes / No
- Stiff Limbs: Do you have difficulty bending or straightening your baby's arms or legs (8)? Yes / No
- Crossed or Stiff Legs: Does your baby's legs cross or stiffen when you pick them up (9)? Yes / No
- Strong: Before two months of age, did your baby hold their bottle on their own? Yes / No
- Grasping: Before two months of age, did your baby grab onto something but couldn't let it go (ex., they could hold their own bottle)? Yes / No
- Head Control: Can your baby hold their head steady while on their tummy or in a supported sitting position (7)? Yes / No
- Eye Movements and Focus: Does your child struggle to focus on objects, follow moving objects with their eyes, or have uncontrolled eye movements? Yes / No
- Arched Back: Does your baby's back or neck seem overextended when lifted (9)? Yes / No
- Posture: At 4 months old or older, have you noticed any unusual posture or difficulty maintaining balance when your child is in a sitting or standing position? Yes / No
- Feeding Difficulties: Does your baby struggle with sucking, swallowing, or coordinating sucking and swallowing (10) or does your baby drool excessively? Yes / No
- Favoring One Side: Does your baby consistently use one hand while keeping the other fisted (8)? Yes / No
- Symmetry in Movement: Have you noticed a lack of symmetry in your child’s movements, such as favoring one side of their body or using one hand significantly more than the other? Yes / No
- Reactions to Stimuli: Does your child seem overly startled by loud noises or does not react to stimuli as expected? Yes / No
- Primitive Reflexes: Does your child exhibit exaggerated reflexes or retain certain reflexes that are usually outgrown in infancy? Yes / No
- Rolling Over: Can your baby roll over in both directions (8)? Yes / No
- Rolling Over: Your baby is rolling over before 2 months of age and the movement appears uncontrolled (31)? Yes / No
- Bringing Hands Together: Can your baby bring their hands together or to their mouth (8)? Yes / No
- Crawling: Does your baby crawl, and if so, is it in a typical manner (11)? Yes / No
- Sitting: Can your baby get into a sitting position and stay seated without support (11)? Yes / No
- Pulling to Stand: Does your baby try to pull themselves up to stand while holding onto furniture (11)? Yes / No (This is a trick answer as either answer could be a warning sign. Pulling to standing is not optimal development. If your child 11 months old or older and not even trying to stand, then you still have non-optimal development and milestone delay)
- Motor Skills Development: Has your child shown delays or been really early in reaching optimal milestones show on our Movement Lesson™ Optimal Development Chart?
The Movement Lesson™ optimal milestones in our Milestone Momentum Chart and their timeline for accomplishment are as follows:
-
Sleeping and Lying Down Milestone - 4 Weeks Old (.9 Months)? Yes / No
-
Tummy Time Milestone - at 8 weeks Old (1.8 Months)? Yes / No
-
Looking at You Milestone - at 12 Weeks Old (2.7 Months)? Yes / No
-
Rolling Over Milestone - at 16 Weeks Old (3.6 Months)? Yes / No
-
Grabbing the Feet Milestone - at 20 Weeks Old (4.6 Months)? Yes / No
-
Independent Sitting Milestone - at 24 Weeks Old (5.5 Months)? Yes / No
-
Coming to Sitting Milestone - at 28 Weeks Old (6.4 Months)? Yes / No
-
Going Into All Fours Milestone - at 32 Weeks Old (7.4 Months)? Yes / No
-
Crawling Milestone - at 36 Weeks Old (8.3 Months)? Yes / No
-
Crawling Reaching Down Milestone - 40 Weeks Old (9.2 Months)? Yes / No
-
Crawling Reaching Up Milestone - 44 Weeks Old (10.1 Months)? Yes / No
-
In and Out of Standing Milestone - 48 Weeks Old (11 Months)? Yes / No
-
Standing With Support Milestone - 52 Weeks Old (12 Months)? Yes / No
-
- Speech and Communication: Is your child delayed in speech development or showing difficulties in communication for their age? Yes / No
The more BLUE answers you have the more likely it is that your child’s movements are organizing to CP. For quick guidance on what to do to start reorganizing your child’s movements towards optimal development, CLICK HERE to join our Facebook Group, post a video and request a FREE movement review.
The Movement Lesson Rule of Thumb: If you are worried about CP, ACT LIKE YOU HAVE IT! BE PROACTIVE AND START GIVING YOUR CHILD MOVEMENT INTERVENTION. CP or not, a baby’s development should never look hard, awkward, stiff, take a lot of effort and so forth. You can only do good if you start intervention now with gentle touch and rotational movements!
Communicating with Your Doctor:
If you notice any of these signs, it's essential to communicate your concerns to your pediatrician clearly and effectively. Here's how to approach the conversation:
- Be Specific: Instead of simply saying "I'm worried about CP," describe the specific signs you've observed. For example, "My baby is 6 months old and still can't roll over in either direction, and they seem to favor their right side all the time." (12)
- Note that when talking with your doctor, you will want to describe the delay in development based on CDC guidelines or the guidelines within the country you live. Deviating a little from the Movement Lesson™ Optimal Development Guidelines, your child will be within the warning parameters of what would be deemed as not-concerning.
- Document Milestones: Keep a record of your baby's developmental progress, noting any delays or concerns. This will help you provide your doctor with a clear picture of your baby's development (12).
- Note that if your concerns are not documented, what concerning thing you saw didn’t happen. VIDEO RECORD EVERYTHING so you can show your doctor what is going on instead of trying to describe to them what is going on! We also recommend that you document things of concern on paper so you can show your doctor how your child’s development is trending. Trending means that over a period of time your child’s development is moving towards or away from a medical warning parameter.
- Ask Questions: Don't hesitate to ask your doctor about their assessment of your baby's development and any recommendations for further evaluation or intervention (12). Ask questions like
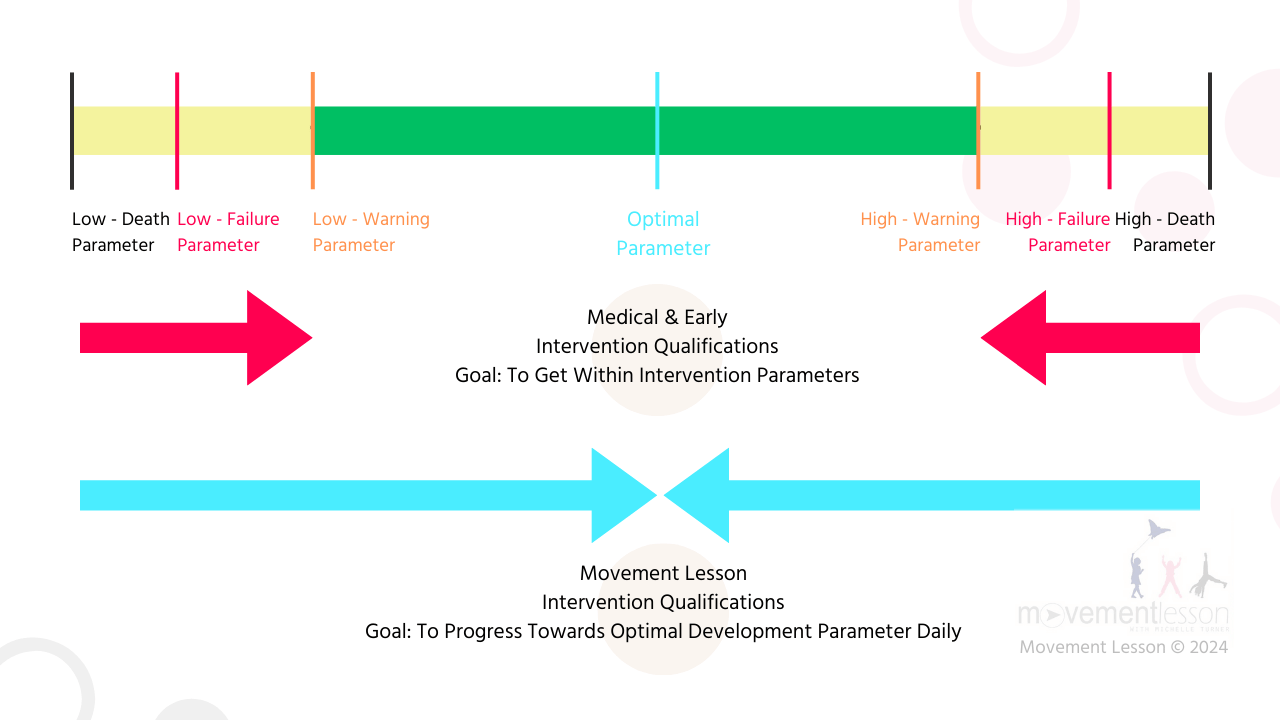
- What are your parameters? warning, failure (emergent), and death
- What is your protocol for CP when these different parameters are hit?
- What kinds of things would make you worried about CP?
- When should I reach out to you if I am seeing the things you are mentioning?
- Advocate for Your Child: If you feel your concerns aren't being taken seriously, don't be afraid to seek a second, third, forth, or 26th opinion or request a referral to a specialist, such as a pediatric neurologist or developmental pediatrician (13).
- Note that even when you push, sometimes you simply can’t get a referral. So you will want to get clear idea of the doctor’s failure parameters or requirements that would prompt him refer your child to these specialists. Again, make sure to take video recordings and to make dated notes on what you are seeing at home if your child’s actions or inactions are trending towards the parameters.
- Note that the parameters trigger protocols or algorithms to your doctor. These are points that a child is PROVING they can’t do something on their own and therefore REQUIRES reactive and often emergency intervention. So if they are saying your child is fine. Your child may not be as fine as you think. As long as you are within the failure parameters, your child will be deemed “fine.” A proactive doctor strives to get your child within the warning parameters. The worst thing is to be blind sided with this thinking that your child is okay and suddenly they are not.
- Short story by Erin Fulks. When in the hospital with one of my kids, I had a daughter who had to be put on life support. In a 1.5 month period we had tried to extubate her three times and before the forth time, the doctors gathered together in a meeting with me to tell me that my daughter was communicating that she may not be able to live on her own. I had two decisions, to either let her pass, or to do a trache. I HAD NO IDEA WE WERE EVEN CLOSE TO THE DEATH PARAMETER! They kept telling me that she was fine and now suddenly she was not fine and could die. Then an there I decided to never be caught unawares of where the warning, failure, and death parameters are. By knowing the parameters I have also learned not to be bitter towards doctors. Again their niche is reactive and emergent care, not proactive, and optimal care. Both sides of the coin are needed and with Movement Lesson, you can become a proactive parent who offers their child optimal movement experiences like me!

How is Cerebral Palsy Diagnosed?
Diagnosing cerebral palsy is a comprehensive process that involves careful observation, medical examinations, and sometimes specialized tests (4). Doctors consider a variety of factors when evaluating a child for cerebral palsy, including:
- Developmental History: Doctors will inquire about the child's developmental milestones, such as when they started rolling over, sitting, crawling, and walking. Any delays or abnormalities in these milestones may be a cause for concern.
- Keep in mind that every milestone will have their parameters. Movement Lesson has one parameter and that's optimal development. When you child is deviating from optimal development regardless of the cause, we want you to start intervening and supporting their optimal development AND KEEP THEIR MOVEMENT AND DEVELOPMENT TRENDING TOWARDS OPTIMAL! For the doctor, they have a range of parameters for each milestone, and each parameter has a warning and failure point. Usually your doctor is looking at how many milestones your child has failed. The more milestones that have been failed, the higher your child is at risk for CP or something else. For many milestones, regardless of their quality, as long as a variation of a milestone has happened within a parametered timeline, your child's development is considered a success.
- At Movement Lesson we call this the "figured it out" mentality. You will be told not to worry and let your child "figure out" development. Again, if your child is deviating from optimal development, their ability to figure things out in the most optimal way is less and less. Figuring things out means a child can come up with a variety of ways to accomplish the same task that the situation demands. If a child only has one way to do something regardless of the situation, then your child is in the "this is the way things are, and I have no choices to make changes" process. So when you are seeing a child that is constantly frustrated, the child is telling you "I can't figure this out and I need help."
- Keep in mind that every milestone will have their parameters. Movement Lesson has one parameter and that's optimal development. When you child is deviating from optimal development regardless of the cause, we want you to start intervening and supporting their optimal development AND KEEP THEIR MOVEMENT AND DEVELOPMENT TRENDING TOWARDS OPTIMAL! For the doctor, they have a range of parameters for each milestone, and each parameter has a warning and failure point. Usually your doctor is looking at how many milestones your child has failed. The more milestones that have been failed, the higher your child is at risk for CP or something else. For many milestones, regardless of their quality, as long as a variation of a milestone has happened within a parametered timeline, your child's development is considered a success.
- Neurological Examination: This examination assesses the child's reflexes, muscle tone, posture, and coordination.
- Medical History: Doctors will review the child's medical records, including any complications during pregnancy or delivery, prematurity, infections, or head injuries.
- Family History: While cerebral palsy is usually not hereditary, doctors may inquire about any family history of neurological conditions.
- Reproductive Health Factors: Maternal health during pregnancy, including infections, exposure to toxins, and other complications, can be relevant to the diagnosis.
- Paternal Health Records: In some cases, paternal health factors may also be considered.
- Apgar Score: This score, assigned to newborns at birth, assesses their overall health and can provide clues about potential neurological issues.
Diagnostic Tools and Tests
In addition to the above factors, doctors may use various tools and tests to aid in the diagnosis of cerebral palsy.
Remember that even for your developmental screenings in other areas of development, you still have parameters for the skill and parameters for the timeline accomplishment of that skill. Never assume, and if the parameters are not defined, ask questions until you are clear where action and inaction will be taken by your professional teams. Also things like Apgar scores, brain scans, MRIs and all the other points above and below are going to have parameters that the doctor is looking at.
PROACTIVE PARENT TIP: ALWAYS REQUEST YOUR MEDICAL RECORDS AND READ THE RESULTS even if your doctor says "everything looks fine." If the parameters are not defined on the results ask for clarification so you can see for yourself if your child is approaching the parameters. And if they are, what do you need to look out for and possibly be prepared for?
- Developmental Screening Tools: Standardized assessments are used to evaluate a child's development in various areas, including motor skills, language, and cognitive abilities.
- Brain Scans: Imaging techniques, such as cranial ultrasound, MRI, and CT scans, can help visualize the brain and identify any structural abnormalities or damage (15).
- Cranial Ultrasound: Uses sound waves to create an image of the brain.
- MRI: Uses magnetic fields and radio waves to produce a detailed image of the brain.
- CT Scan: Uses X-rays to create a cross-sectional image of the brain.
- Electroencephalogram (EEG): Measures the electrical activity in the brain and can be helpful in diagnosing seizures or other neurological conditions.
- Genetic Testing: May be used to identify genetic abnormalities that could contribute to cerebral palsy.
- Metabolic Testing: Assesses the body's chemical processes and can help rule out metabolic disorders that may mimic cerebral palsy.
When Will a Doctor Start the Diagnosis Process?
Doctors may suspect CP if they observe developmental delays, abnormal muscle tone, or unusual postures (7). While a diagnosis can sometimes be made as early as 6 months, it often takes until 12-24 months for a definitive diagnosis (8). This is because some signs may be subtle, and doctors want to avoid misdiagnosis (17).
6 months, 12-24 months, these are timeline parameters for proved failure. You child is proving that they can't reach milestones and therefore qualify for reactive support and early intervention services.
For optimal development, these are "later" and "have to" intervention services.
To us, early intervention services mean before a problem manifests; to prepare a system with best compensation skills regardless of the challenges that lie ahead. With Movement Lesson, you can start intervention NOW and help your child's movement and development trend towards optimal functioning. You start taking steps forward by rebuilding their foundational movements in development from the beginning.
If you child is older and you are reading this blog, you can make up for lost time and go back and put in the developmental movements your child missed out on, so there current development optimizes!
How Much Delay Does a Child Need to Have?
There's no specific amount of delay that automatically triggers a CP diagnosis. Doctors consider the overall pattern of development, the presence of other signs, and the results of various assessments (18).
At Movement Lesson, any delay is too much delay; CP or not. You don't need a diagnosis to help your child thrive. If you are worried, start helping your child. We help and teach parents how to do that regardless of how big or how small a parent's worry is.
When Medical Help May Not Be Offered:
If your child's delays are mild or there are no other concerning signs, your doctor may recommend monitoring their development and providing guidance on activities to promote development at home (17).
At Movement Lesson we call this the “wait and see” approach. The medical field’s niche is reactive and emergent care. It’s necessary, but unless something is an emergency, your child goes on a waiting list and the hope is that they figure things out and that they don’t need intervention services after all. Waiting lists can be 6 to 12 months out.
Believed Benefits of Traditional Early Intervention
Early intervention plays a vital role in supporting the development of children with cerebral palsy. Research highlights the numerous benefits of early intervention, including:
- Maximizing Neuroplasticity: A child's brain exhibits remarkable plasticity, particularly in the first few years of life. This means the brain has a greater capacity to adapt and rewire itself in response to experiences and learning. Early intervention capitalizes on this neuroplasticity to promote optimal brain development and improve motor function (19).
- Minimizing Secondary Impairments: Cerebral palsy can lead to secondary impairments, such as muscle stiffness, joint contractures, and skeletal deformities. Early intervention helps prevent or reduce these complications by promoting proper movement patterns and providing appropriate support (20).
- Improving Motor Skills: Early intervention programs often incorporate physical therapy, occupational therapy, and speech therapy. These therapies help children develop essential motor skills, improve coordination, and enhance communication abilities (20).
- Supporting Cognitive and Social-Emotional Development: Early intervention provides opportunities for learning, interaction, and play, which are crucial for cognitive and social-emotional development. Children who receive early intervention are often better equipped to manage frustrations stemming from physical limitations, experience a greater sense of achievement as they develop new skills, and develop emotional resilience (21).
- Enhancing Quality of Life: By addressing the challenges of CP early on, early intervention can help children achieve their full potential and lead more independent and fulfilling lives (21).
Believed Benefits of Early Physiotherapy
Early physiotherapy interventions are particularly valuable in promoting motor development and preventing complications. These interventions can:
- Improve cardiovascular fitness (22)
- Improve muscle activation and strength (22)
- Improve motor control (22)
- Improve effectiveness and variability of movement (22)
- Preserve muscle length and joint flexibility (22)
The Importance of Active Movement
Neuroscience research emphasizes the critical role of early active movement in brain development. Infants who are not actively using their motor cortex risk losing cortical connections and dedicated function (23). Early intervention and therapeutic activities that encourage active movement are essential for promoting healthy brain development and motor function.
Believed Benefits of Movement Lesson Early Intervention
With Movement Lesson early intervention starts day one of birth. (A highly advanced Movement Lesson Practitioner can start early intervention in utero.) Our mission is to eradicate special needs where it can be avoided. Our mission is to give children with special needs the experiences of optimal development so they can choose their best future. Here are the highlights the numerous benefits of Movement Lesson early intervention, including:
- Rotational Movements in Opposition to Gravity: The one thing a child with Cerebral Palsy has in common with any other developmentally delayed child is lack of rotational movements. Lack or rotational movements make gravity a heavy force in the system. That's why therapies think that by making the body stronger it will move better in gravity and therefore develop. This approach actually wears the system down faster. Rotational movements cancel out gravity and, like a fish floats in water, when we float in gravity optimal development just happens.
- Quantum Mapping: The step before neuromapping. Quantum Mapping implies that quantum processes lay the groundwork for the brain's subsequent control of movement. This involves:
- Establishing a Quantum "Blueprint": Quantum mapping creates a coherent quantum state throughout the body, encoding information about the body's structure, function, and intended development.
- Facilitating Communication: Quantum entanglement and information processing enables rapid and efficient communication between different parts of the body, preparing the system for the brain's signals and neurological processing.
- Priming the Nervous System: Quantum processes influences the state of the nervous system, making it more receptive to the brain's signals and facilitating the initiation and coordination of a multitude of simultaneous movements with exact precision. Every cell, even every atom, in the body must know it's purpose in function in relationship to the body as a whole and must initiate first rotational movements independent of the brain and then be stimulated and enhanced by the neurological processes of the brain.
- Traditional and other alternative modalities assume the brain can just rewire itself to optimal when it can't. It can only rewire itself to the underlying quantum blueprint that exists for rotational movements. The rewiring will stop if the quantum blueprint is maxed out. Which we call a rotational movement threshold. If a quantum blueprint can be maxed out that means a person has "fixed" neuroplasticity.
- Fixed neuroplasticity is the brain's tendency to solidify frequently used neural pathways into rigid patterns, leading to efficient but potentially inflexible movement and limited adaptability. This can hinder the exploration of new movement possibilities and optimal development.
- Movement Lesson works to create a new quantum blueprint so there is no "maxing out." When you do a movement lesson your intent is to give the body the movement structure and function needed for optimal development. As a result, fixed neuroplasticity is replaced with 6 new types of neuroplasticity that create the dynamic, adaptive, responsive, fluid, interactive, and generative we are used to seeing in a healthy system. This is what takes the body off the path of non-optimal development and puts it onto the path of optimal development.
- Fixed neuroplasticity is the brain's tendency to solidify frequently used neural pathways into rigid patterns, leading to efficient but potentially inflexible movement and limited adaptability. This can hinder the exploration of new movement possibilities and optimal development.
- Traditional and other alternative modalities assume the brain can just rewire itself to optimal when it can't. It can only rewire itself to the underlying quantum blueprint that exists for rotational movements. The rewiring will stop if the quantum blueprint is maxed out. Which we call a rotational movement threshold. If a quantum blueprint can be maxed out that means a person has "fixed" neuroplasticity.
- Maximizing 6 Types of Neuroplasticity:
-
1. Dynamic Neuroplasticity: This emphasizes the ongoing, active nature of the brain's changes, highlighting that it's not a one-time event but a continuous process.
-
2. Adaptive Neuroplasticity: This explicitly connects neuroplasticity to the concept of adaptation, making it clear that the brain's changes are driven by the need to respond to environmental demands.
-
3. Responsive Neuroplasticity: Similar to "adaptive," this emphasizes the brain's ability to react and adjust to changes in the environment, highlighting its sensitivity and flexibility.
-
4. Fluid Neuroplasticity: This evokes a sense of flexibility and continuous change, suggesting that the brain's structure and function are constantly flowing and adapting.
-
5. Interactive Neuroplasticity: This highlights the interplay between the brain and the environment, emphasizing that neuroplasticity is not just an internal process but a dynamic interaction with the world.
-
6. Generative Neuroplasticity (GN): This term captures the idea that neuroplasticity doesn't just allow the brain to react to the environment, but to actively create new possibilities. It implies that the brain's dynamic, adaptive, and responsive qualities ultimately lead to the generation of new skills, abilities, and even ways of thinking.
- GN encompasses the active nature: It goes beyond simply adapting; it suggests the brain is actively producing something new if the quantum mapping is there to do so.
- GN highlights the creative potential: It implies that neuroplasticity isn't just about fixing problems or responding to challenges, but about exploring new possibilities and generating novel solutions if the quantum mapping is there to do so.
- GN reflects the evolving nature of the brain: It captures the idea that the brain is constantly growing and developing, generating new connections and capabilities throughout life if the quantum mapping is there to do so.
-
Optimal Movement, Development, and Independence for Best Quality of Life
The one thing proactive parents need is an action plan that tells them exactly where there child is at in development, what developmental pieces are missing, and what can be done at home on a daily basis to create the missing parts of movement so development can happen and a child can achieve their ultimate independence. Lastly you need a way to recognize when developmental optimization is happening. Movement Lesson teaches parents how to recognize developmental optimization in fine and gross motor skills, vision, language and development, cognitive, sensory, and emotional development with Cerebral Palsy, or with any type of diagnosis or non-diagnosis.
Traditional Plan of Action Following a Cerebral Palsy Diagnosis
When a child receives a cerebral palsy diagnosis, a team of healthcare professionals collaborates with the child and family to create a personalized plan of action. This plan typically includes a combination of therapies, interventions, and support services:
- Therapies:
- Physical therapy: Focuses on improving motor skills, strength, balance, and coordination through exercises and activities (24).
- Occupational therapy: Helps children develop skills for daily living, such as dressing, eating, and playing, by adapting tasks and environments (24).
- Speech therapy: Addresses communication difficulties, including speech production, language comprehension, and alternative communication methods. It also helps manage swallowing difficulties (25).
- Medications: May be used to manage muscle stiffness, spasticity, and other associated conditions, such as seizures or pain (26).
- Assistive Devices and Technology: Can include wheelchairs, walkers, orthotics, communication devices, and adaptive equipment to support mobility, communication, and independence (24).
- Surgery: In some cases, surgery may be necessary to correct bone deformities, reduce muscle spasticity, or improve function. Surgical options may include tendon lengthening, muscle releases, or spinal surgery (26).
- Early Intervention Programs: Provide comprehensive services to support the child's development in various areas, including motor skills, communication, and cognitive abilities. These programs also offer resources and support for families (13).
The Movement Lesson™ Optimal Plan of Action For Risk of Cerebral Palsy or CP Diagnosis
- Step 1: Decide that you will do everything in your power to learn how to optimize your child's development by giving the gift of movement with daily movement lessons.
- Step 2: Start at the beginning with our FAST START program (CLICK HERE to learn more). No matter your child's age their development will only be as good as their first milestone movements. With Movement Lesson you can give the body the experiences of infant milestone movements and put them on a new path of developmental optimization.
- Step 3: Create the milestone momentum needed for optimal movement, development and independence. How? It sound's intimidating, but we make it easy with simple step-by-step exercises that are intuitive, technical, and play based. We also have diagrams to help you know what to think and do while applying the exercises.
- Step 4: Create a schedule for doing daily exercises and do the exercises even when you don't want to. When you feel uncertain about what you are doing or what impact you are having, consult with a Movement Lesson Practitioner so they can teach you how to work through and learn from your road blocks. In our Fast Start Program you get FREE 1-on-1s with a Movement Lesson Practitioner so we can help you stay successful in your home application of the exercises.
- Step 5: Believe it's possible to help your child become their best self by giving them the gift of movement. Believe, go all in, and never look back!
- Step 6: See your child's development as optimal. As you focus on this, you will your movements optimize is big and small ways.
Things Parents Can Do NOW to Help Their Child Thrive
Especially when your child doesn't qualify for early intervention services, there are many things you can do to support their development:
- Give Your Child a NEW Breathing Foundation: Even if you think your child is breathing fine, children with CP have a compromised quantum blueprint of their breath structure. If the body has to work at maintaining breathing, balance, and/or heart functions, it will not work on optimizing developmental movements.
- Get 60 Day Free Access to our FAST START OPTIMAL DEVELOPMENT PROGRAM which has our breathing course in it. Start doing the exercises for at least 15 minutes a day, and observe for developmental optimization. You know developmental optimization is happening when movement becomes easier, looks more fluid, or looks more coordinated, you see your child do new things today that they weren't doing yesterday; your child can be more sleepy for a short time, and then have an increase in energy and stamina and so on. CLICK HERE to learn more and get started.
- Encourage Active Movement: Provide opportunities for tummy time, reaching for toys, and exploring different movements (23). Don't swaddle, stop using containers except when necessary and for safety. Take your baby out of the carseat when you go shopping or out to eat or, when possible, when they are sleeping. Doing these things can make child care seem harder, but your child needs their body to learn movement in a natural way, and if you are not giving them natural movement experiences you are going to have to learn the technicalities of movement and development through our programs.
- Create a Stimulating Environment: Offer a variety of toys and activities that engage your child's senses and encourage exploration. Your child's best toy is your face and interacting and engaging with you. Reduce the amount of black and white you use and keep the environment simple.
- Read and Sing to Your Child: This promotes language development and cognitive skills.
- Provide Love and Support: Create a nurturing and supportive environment where your child feels safe and loved.
- Connect with Other Parents: Join support groups or online communities to connect with other parents of children with CP or developmental delays (27).
Resources for CP Parents
Navigating a cerebral palsy diagnosis can be overwhelming. Fortunately, there are numerous organizations and resources dedicated to supporting families and individuals with CP:
- Cerebral Palsy Foundation (CPF): Focuses on research, innovation, and public awareness to improve the lives of those with cerebral palsy (28). They offer resources, information, and support for families.
- United Cerebral Palsy (UCP): Offers a wide range of services and support to individuals with cerebral palsy and their families, including therapy services, advocacy, and community living programs (28).
- March of Dimes: Supports research and programs that benefit infants and children with disabilities, including cerebral palsy (28). They provide information, resources, and support for families.
- The Cerebral Palsy Alliance: Provides therapies, life skills programs, equipment, and research funding related to cerebral palsy (28). They offer a variety of services to support individuals with CP throughout their lifespan.
- CP NOW Foundation: Offers extensive information about diagnosis, treatment decisions, and resources for daily life (29). They provide resources and support for families navigating the challenges of CP.
- Child Neurology Foundation: Provides support to parents and caregivers of children with a neurologic diagnosis, including cerebral palsy (29). They offer information, resources, and support groups.
- Cerebral Palsy Family Network (CPFN): The world's largest online community for connecting and supporting families impacted by cerebral palsy (27). They provide a platform for families to share experiences, find information, and connect with others.
- MyChild: Offers comprehensive resources for parents and other caregivers of children with cerebral palsy and other neurological conditions (30). They provide information, support, and connections to resources.
Conclusion
Early detection of cerebral palsy is paramount. By being aware of the potential warning signs and seeking prompt medical attention, parents can play a proactive role in their child's development. While cerebral palsy presents unique challenges, early intervention can significantly improve a child's motor skills, cognitive abilities, and overall quality of life. Remember that a variety of resources and support systems are available to help families navigate this journey. With the right interventions and a supportive network, children with cerebral palsy can thrive and reach their full potential.
Works Cited
- Cerebral Palsy (CP) Information | Diagnosis, Causes, & Treatment, accessed January 1, 2025, https://www.cerebralpalsyguidance.com/cerebral-palsy/
- www.ninds.nih.gov, accessed January 1, 2025, https://www.ninds.nih.gov/health-information/disorders/cerebral-palsy#:~:text=Cerebral%20palsy%20(CP)%20refers%20to,body%20movement%20and%20muscle%20coordination.
- Cerebral Palsy | National Institute of Neurological Disorders and Stroke, accessed January 1, 2025, https://www.ninds.nih.gov/health-information/disorders/cerebral-palsy
- Diagnosis of Cerebral Palsy | Testing for CP - CerebralPalsy.org, accessed January 1, 2025, https://www.cerebralpalsy.org/about-cerebral-palsy/diagnosis
- Cerebral palsy - Symptoms and causes - Mayo Clinic - Guardian Ad Litem, accessed January 1, 2025, https://guardianadlitem.org/wp-content/uploads/2018/01/Cerebral_Palsy1.pdf
- Cerebral Palsy: An Overview - AAFP, accessed January 1, 2025, https://www.aafp.org/pubs/afp/issues/2020/0215/p213.html
- Cerebral Palsy Symptoms | Signs of Cerebral Palsy | Cerebral Palsy Alliance Australia, accessed January 1, 2025, https://cerebralpalsy.org.au/cerebral-palsy/signs-symptoms/
- Cerebral Palsy Symptoms | Birth Injury Center, accessed January 1, 2025, https://birthinjurycenter.org/cerebral-palsy/symptoms/
- Cerebral Palsy Symptoms & Signs in Newborn Babies, accessed January 1, 2025, https://www.cerebralpalsyguide.com/cerebral-palsy/symptoms/
- Cerebral palsy – Symptoms - NHS, accessed January 1, 2025, https://www.nhs.uk/conditions/cerebral-palsy/symptoms/
- What are the early signs of cerebral palsy? | NICHD - National Institute of Child Health and Human Development, accessed January 1, 2025, https://www.nichd.nih.gov/health/topics/cerebral-palsy/conditioninfo/signs
- Cerebral palsy - Diagnosis and treatment - Mayo Clinic, accessed January 1, 2025, https://www.mayoclinic.org/diseases-conditions/cerebral-palsy/diagnosis-treatment/drc-20354005
- Treatment and Intervention for Cerebral Palsy - CDC, accessed January 1, 2025, https://www.cdc.gov/cerebral-palsy/treatment/index.html
- Cerebral palsy | NHS inform, accessed January 1, 2025, https://www.nhsinform.scot/illnesses-and-conditions/brain-nerves-and-spinal-cord/cerebral-palsy/
- Cerebral palsy – Diagnosis - NHS, accessed January 1, 2025, https://www.nhs.uk/conditions/cerebral-palsy/diagnosis/
- Early Signs of Cerebral Palsy in Newborn Babies - Birth Injury Lawyers Alliance, accessed January 1, 2025, https://www.bila.ca/birth-injuries/cerebral-palsy/signs/
- Diagnosing Cerebral Palsy - Getting a Proper Diagnosis, accessed January 1, 2025, https://www.cerebralpalsyguide.com/cerebral-palsy/diagnosis/
- Diagnosing Cerebral Palsy in Children - NYU Langone Health, accessed January 1, 2025, https://nyulangone.org/conditions/cerebral-palsy-in-children/diagnosis
- Early Intervention for Cerebral Palsy: Examples & What to Do - Flint Rehab, accessed January 1, 2025, https://www.flintrehab.com/cerebral-palsy-early-intervention/
- Early Intervention Therapy - Cerebral Palsy Alliance, accessed January 1, 2025, https://cerebralpalsy.org.au/wp-content/uploads/2023/06/CPA18_EarlyInterventionGuide_LR.pdf
- 5 Benefits of Early Intervention for Children with Cerebral Palsy - Medbridge Blog, accessed January 1, 2025, https://www.medbridge.com/blog/2024/11/5-benefits-of-early-intervention-for-children-with-cerebral-palsy/
- Early Intervention in Cerebral Palsy - Physiopedia, accessed January 1, 2025, https://www.physio-pedia.com/Early_Intervention_in_Cerebral_Palsy
- Early Detection of Cerebral Palsy - AACPDM, accessed January 1, 2025, https://www.aacpdm.org/publications/care-pathways/early-detection-of-cerebral-palsy
- What are common treatments for cerebral palsy? | NICHD - National Institute of Child Health and Human Development, accessed January 1, 2025, https://www.nichd.nih.gov/health/topics/cerebral-palsy/conditioninfo/treatments
- What Are The Treatment Options? - Cerebral Palsy Guide, accessed January 1, 2025, https://www.cerebralpalsyguide.com/treatment/
- Cerebral palsy – Treatment - NHS, accessed January 1, 2025, https://www.nhs.uk/conditions/cerebral-palsy/treatment/
- Cerebral Palsy Family Network | Cerebral Palsy Resources | CPFN, accessed January 1, 2025, https://cpfamilynetwork.org/
- Cerebral Palsy Support Groups | Find Valuable CP Resources, accessed January 1, 2025, https://www.cerebralpalsyguide.com/community/
- Cerebral Palsy Resources for Families | St. Louis Children's Hospital, accessed January 1, 2025, https://www.stlouischildrens.org/conditions-treatments/cerebral-palsy-center/resources-for-families
- Cerebral Palsy Resources - National Institute of Child Health and Human Development, accessed January 1, 2025, https://www.nichd.nih.gov/health/topics/cerebral-palsy/more_information/resources
-
When do babies roll over? Factors, support, and timeline - MedicalNewsToday, accessed January 12, 2025, https://www.medicalnewstoday.com/articles/when-do-babies-roll-over
